A simple algorithm for differential diagnosis in hemodynamic shock based on left ventricle outflow tract velocity-time integral measurement
Simple algorithm based on left ventricle outflow tract (LVOT) velocity time integral for differential diagnosis in hemodynamic shock proposed by the Spanish Critical Care Ultrasound Network Group.
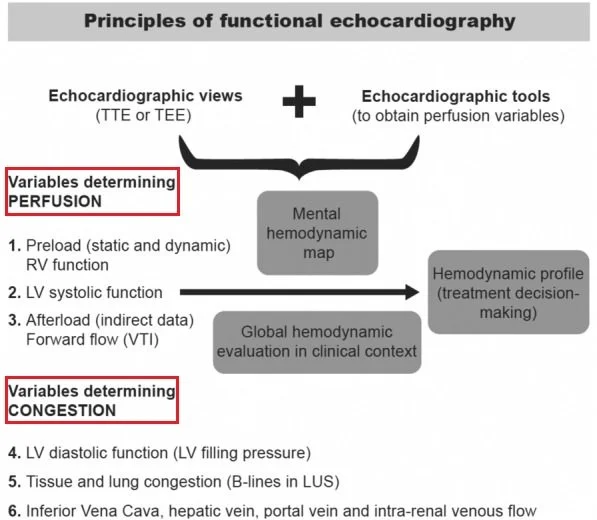
Assessment of hemodynamic status is based on two concepts: perfusion and congestion.
Congestion may be assessed by lung ultrasound as well as, hepatic, portal vein and venous renal congestion (VEXUS Score) along with trans-mitral inflow and E/e’ ratio to estimate LV filling pressures.
Measuring forward flow, by LVOT velocity–time integral measurement, in the LVOT or right ventricle outflow tract (RVOT), which will allow us to measure variables related to perfusion (preload, afterload and contractility). This variable integrated into clinical context may have a potential role in the differential diagnosis for hemodynamic shock in critically ill patients.
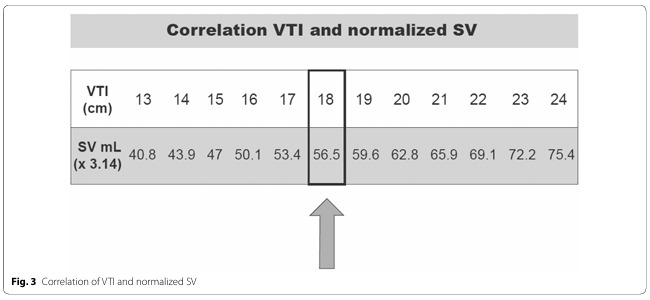
SV may be calculated based on VTI values. A calculated VTI of 18 cm, corresponds to an SV of 56.5 mL, which is very close to 60 mL, which is the lower limit of normality, according to hemodynamic literature and the cut-off value to define a low SV.
First step is to analyze whether the patient has an adequate forward flow in terms of SV and CO :
If the LVOT VTI is above 0 cm, the SV is adequate and therefore the cause of the hemodynamic shock will most likely be a distributive shock. In this case, after initiating vasopressors to normalized mean blood pressure, VTI will be reassessed to ensure SV has not been
reduced by increasing afterload related to vasopressors.
If VTI is below 16 cm, an abnormally low SV is suggested, and the cause of this lowcardiac output syndrome should be diagnosed.
(The lower limit of VTI has been downgraded to 16 cm because most of the time in critical care, images obtained are less than optimal and there is a tendency to underestimate the VTI, due to a suboptimal Doppler bean alignment).
The order followed for the perfusion parameters assessment in the algorithm is not trivial. The goal is to recover perfusion parameters without over resuscitating the patient avoiding adverse effects. For this reason, fluid responsiveness is the last one to be evaluated, after ruling out tamponade, RV/LV systolic function and left-sided valvular incompetency.
About LVOT VTI @ HCP Rounds
Thanks to the authors.