Fever in sepsis revisited : is a little heat what we need ?
Fever = coordinated rise in temperature in response to infectious and noninfectious causes, which varies with the anatomical site.
Adaptive heat shock response < millions of years in vertebrates !
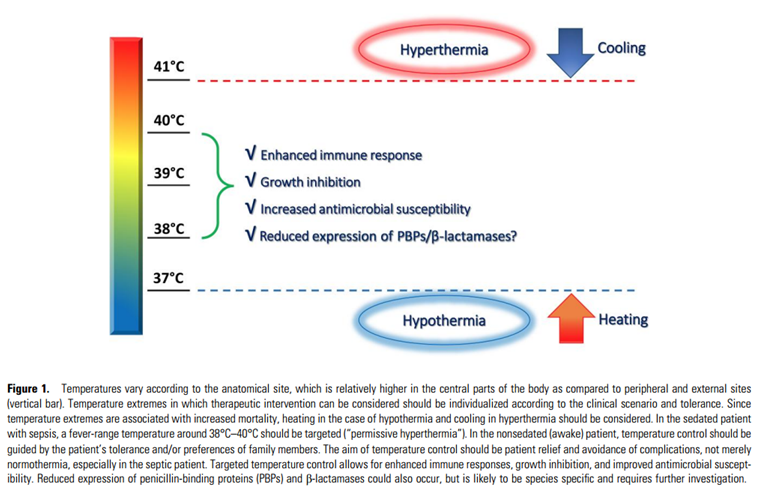
Elevated temperature stimulates and optimizes innate and adaptive immune responses. In addition, most microorganisms have shown thermal stress–related growth inhibition, and in vitro data indicate that β-lactam antibiotics in particular appear to have significantly improved susceptibility profiles in the presence of fever-range temperatures.
Favorable effects of fever but many physicians consider fever a harmful event that should be treated without discrimination of the underlying cause.
Observational studies have indicated that attempts to lower the temperature in patients with sepsis are associated with increased mortality.
Diagnosis and management of temperature abnormalities vary widely among ICUs.
Oral or rectal temperatures are preferred over other less reliable measurement methods (eg, axillary or tympanic membrane temperatures). The anatomical site of the temperature measurement should be noted and remain consistent to allow for accurate comparison.
Pharmacological treatment is preferred over nonpharmacological treatment.
The current Surviving Sepsis Guidelines do not make recommendations on how to manage fever ==> a 2023 SCCM guideline about new fever in the adult ICU patient states : “For critically ill patients with fever, we suggest avoiding routine use of antipyretic medications for the specific purpose of reducing the temperature (weak recommendation, moderate quality evidence).” In addition, “for critically ill patients with fever who value comfort by reducing temperature, we suggest using antipyretics over nonpharmacologic methods to reduce body temperature (weak recommendation, low-quality evidence)” [ref]. Importantly, in the guideline, no differentiation is made between septic and nonseptic critically ill patients.
Conclusion : based on preclinical and clinical data, a “permissive hyperthermia” allows for bacterial growth inhibition, enhanced immune responses, and increased antimicrobial susceptibility. Fever-range temperatures are beneficial for the septic patient therefore fever in sepsis should be managed in an individualized manner.